When Is Back Pain a Spinal Compression Fracture?
If you experience back pain, you are not alone – 80 percent of people will suffer from it at some point in their life. While it typically lasts a few days to a few weeks and can be managed with at-home care, other aches can be indicative of a more serious issue, such as a spinal compression fracture.

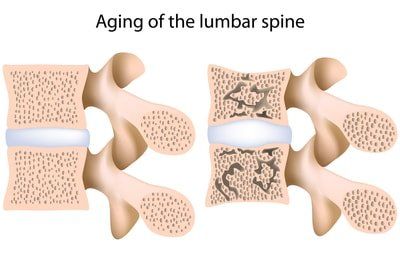
Compression fractures are caused by osteoporosis or spinal trauma. As we get older, our vertebrae wear out and become flatter. If too much pressure is placed on a weakened vertebra, it cracks and causes a fracture. This is often the result of a fall but people with osteoporosis can also suffer a fracture when doing everyday activities, such as coughing, reaching and twisting.
Types of Spinal Compression Fractures
There are several types of compression fractures caused by osteoporosis, such as:
- Wedge –
The
fracture collapses the bone in the front of the spine and leaves the back of
the bone unchanged, resulting in a wedge-shaped vertebra.
- Crush –
The
entire bone breaks.
- Burst –
The
fracture involves some height loss in the front and back walls of the vertebral
body.
Symptoms of Spinal Compression Fractures
A compression fracture causes acute back pain, usually near the damaged vertebra. The pain often increases with movement, especially when you change positions. Other symptoms include :
- Limited spinal mobility
- Eventual decrease in height
- Spinal deformity and disability
Severe pain typically lasts four to six weeks as the bone heals, after which many patients say they experience chronic, achy pain for weeks or months.
Diagnosing a Spinal Compression Fracture
If you have osteoporosis and are suddenly experiencing back pain, it is important to get an accurate diagnosis to prevent further health issues, such as continued pain, decreased physical function and even a higher risk of death.
However, diagnosing a compression fracture is not as straightforward as other conditions. Reasons for this include:
- Assumptions
about pain –
When an older adult complains of back pain, it is often
assumed to be a normal side effect of the aging process. If this occurs, they
may not be checked for a vertebral fracture.
- Harder to
see on an x-ray –
Unlike osteoporosis-related hip or wrist fractures,
spinal compression fractures are more likely to be missed on a standard x-ray.

Your doctor will perform a physical exam and order diagnostic tests, such as a CAT or MRI scan, to determine if you have a compression fracture. They may also ask questions, such as:
- When did the pain start?
- How intense is the pain?
- Where is the pain located?
- Which activities or positions worsen the pain?
- Does the pain radiate to other parts of the
body?
Spinal Compression Fracture Treatment
Compression fracture treatment is often a two-pronged approach that includes caring for the fracture and treating the osteoporosis.
-Nonsurgical Fracture Treatment
Depending on the severity of the fracture, you may be able to help it heal without surgery. Pain management may include:
- Activity
modification –
Your doctor may recommend a few days of bed rest, but
prolonged inactivity may lead to further bone loss and a higher risk for future
fractures.
- Back
bracing –
A brace limits the motion of the fractured vertebra, which can
help reduce pain. Back braces should only be used under a doctor’s supervision
to prevent muscle weakening.
- Medication
–
Carefully prescribed pain medications can help relieve aches.
Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are commonly
recommended, as they carry a lower risk for addiction than narcotics and muscle
relaxants.

-Surgical Fracture Treatment
When chronic pain persists, surgery may be the option of last resort. There are three surgical procedures used to treat compression fractures:
- Vertebroplasty
–
Your surgeon inserts a needle in your spine to inject the damaged
vertebra with a bone cement mixture.
- Kyphoplasty
–
A catheter tube with a balloon on one end is used to put liquid cement
into the vertebra.
- Spinal
fusion –
Metal screws are placed through a small tube into the vertebra and
metal plates or rods are bolted together in the back of the spine to hold the
vertebrae in place.
-Osteoporosis Treatment
After experiencing a compression fracture, patients are at a higher risk for additional fractures if their osteoporosis is not properly managed. Treatment typically involves a combination of:
- Calcium and vitamin D supplements
- Hormone replacement therapy for women
- Weight-bearing exercises
Compression Fracture Treatment in Central Georgia
When treating your compression fracture at home does not relieve your pain, minimally invasive procedures like kyphoplasty can help. The physicians at Vascular & Interventional Radiology Associates of Central Georgia (VIRA) have performed thousands of these surgeries with excellent results. Our team will work with you to help you get back to living pain-free. Call 478-757-8868 or schedule your appointment online.